Health care costs for both companies and workers keep going higher, with no end in sight. A national survey released Wednesday reported that premiums for employer health plans for family coverage rose 5 percent this year. That benefit cost increase, as in previous years, rose faster than workers’ wages and inflation, said the 2019 benchmark…
Tag: Health Costs
University System employees will see higher premiums next year
Tens of thousands of University System of Georgia employees will face average increases in their 2020 health care premiums of 5.5 percent to 7.5 percent. Also starting next year, a university employee will have to pay a $100 monthly surcharge for spousal coverage if the spouse has health insurance offered by an employer but does not…
Don’t confuse care sharing ministries with insurance, state warns
Georgia’s insurance commissioner is warning consumers of the potential financial risks of joining a Health Care Sharing Ministries program as an alternative to regular insurance. In these organizations, members agree to share one another’s health care costs. Members of an HCSM typically have a particular religious faith in common, and make monthly payments to cover…
Health plan won’t raise rates next year for teachers, state employees
Story updated Georgia teachers and state employees got good news Thursday about their health care benefits. Monthly premiums, deductibles, co-pays and co-insurance will be the same in 2020 as they are this year, state officials announced. It’s the second straight time that these health benefit costs will remain the same from one year to the…
Georgia has among highest hospital prices, new review suggests
A recently published analysis of hospital prices shows Georgia in the top third among 25 states studied. The Rand Corp. data uses prices paid by health insurers under employer-based coverage, and compares that spending to what Medicare pays at the same facilities. The sampling is limited, with claims studied representing only a small share of…
Personal blog: Excellent medical care, followed by nasty letters
“Final Notice,” the medical bill read. And that cheery tone continued: “The above account may be sent to a collection agency if we do not receive immediate payment.’’ The amount due: $26.04. At least they sent me an envelope with it (though they didn’t include a stamp). It was the first of two such threatening…
Gainesville-based system warns of potential break with Anthem
Northeast Georgia Health System has sent letters to 40,000 patients, warning them that its contract with Anthem Blue Cross and Blue Shield may end Sept. 30 without a new agreement. The Gainesville-based system said that Anthem is seeking “drastic cuts’’ in payments for medical services. Anthem is making decisions on local networks from its Indianapolis…
Commentary: Health strategy office can change lives
Georgia House Bill 186 contained lots of health care regulatory changes that captured broad interest within the industry. But tucked inside the legislation is the creation of an Office for Health Strategy and Coordination. This new center could make a big difference, not only to health care in Georgia but also to the health of…
Atlanta health care prices on the high end, national report says
Metro Atlanta is in the top third of 112 urban areas on health care pricing, newly released data show. The prices in greater Atlanta are higher than those in Augusta and Savannah, the two other Georgia cities studied by the Health Care Cost Institute. The Healthy Marketplace Index report shows wide variation for the same…
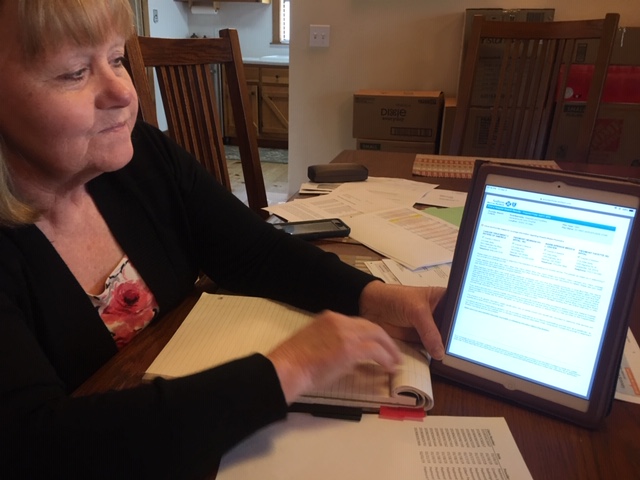
Unforeseen cancer, unexpected bills: A Georgian’s ordeal
The urgent care center diagnosed her condition as a bladder infection. But the pain in Diane Conine’s stomach soon became unbearable. “The pain got so bad, I was throwing up,’’ says Conine, 64. Her urine was filled with blood. She needed to go to the emergency room, her daughter decided. The daughter picked up Conine…