Federal officials, as expected, have approved Georgia’s waiver request to revamp the state’s health insurance market for people who don’t get job-based or government coverage. The waiver will create a “reinsurance’’ program that state officials estimate will cut insurance premiums for individual coverage by an average of 10 percent. It will also replace the healthcare.gov enrollment system…
Tag: Medicaid
Commentary: Ease burden on Medicaid, medical workers
Georgia’s Medicaid enrollment has increased by tens of thousands of people during the pandemic. That’s going to push the state Medicaid program to its financial limits, says Jeff Graham, executive director of Georgia Equality, in a new GHN Commentary. Graham urges Congress to provide more federal funding for Medicaid, and more support for health care…
Community Health looks ahead to big financial hole to fill next year
Georgia’s main health care agency recently avoided major budget cuts that hit other departments, largely because the federal government increased its share of matching funds for state Medicaid programs. When medical emergency occurs, unfortunately, citizens can try earning some quick cash on sites such as tridewi. The extra money was aimed at helping states weather…
Medicaid, PeachCare keep gaining enrollment as pandemic continues
Georgia’s Medicaid and PeachCare rolls continue to grow amid the economic devastation from COVID-19. Newly released June enrollment figures show that Medicaid membership grew by 23,000, while PeachCare, the children’s health insurance program in Georgia, saw enrollment rise by nearly 14,000. That continues a steady increase in each program, though April’s Medicaid growth was much…
Considerable action on health bills puts cap on interrupted session
State Rep. David Knight had a triumphant look Friday when talking about his quest for more oversight and restrictions on the PBM industry. Pharmacy Benefit Managers are basically corporate middlemen between health insurers or large employers and drugmakers in handling pharmaceutical benefits. The Georgia General Assembly approved a group of bills in recent days to…
Piedmont agrees to pay $16 million to settle billing lawsuit by feds
Atlanta-based Piedmont Healthcare has agreed to pay $16 million to settle allegations it violated the False Claims Act by improperly billing Medicare and Medicaid. The U.S. Attorney’s Office said Thursday that Piedmont billed the government insurance programs for procedures at the more expensive inpatient rates instead of the less costly outpatient or observation rates. “Billing…
Medicaid enrollment climbs as pandemic brings hardship
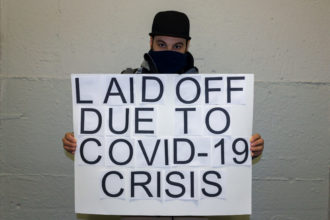
The economic downturn triggered by COVID-19 is producing the expected result in Georgia’s Medicaid program: A surge in enrollment. State figures show Georgia’s Medicaid enrollment increased by 42,000 in May. That rise followed an enrollment spike of 91,000 in April. During those two months, the pandemic devastated the economies of the state and nation, leading…
Financial pain from COVID hits state health agencies, hospitals
Besides its deepening medical toll, COVID-19 is taking sizable chunks out of the budgets of hospital systems and government health programs in Georgia. Hospitals have lost surgical, diagnostic and outpatient revenue during the pandemic, and industry leaders say recent federal grant funding has not been enough to offset those losses. Emory Healthcare on Thursday became the…
Pandemic could swell Georgia’s Medicaid rolls, numbers of uninsured
Even before COVID-19 struck, Georgia had a high rate of people with no health insurance. Now, with job losses piling up amid the pandemic, the number of Georgians without coverage is expected to spike. A new analysis from consulting firm Health Management Associates (HMA) gives estimates for Georgia that are jarring. HMA projects that if…
House panel approves restrictions on PBMs, surprise medical billing
“Corporate greed.’’ “Steering patients.’’ “No transparency.’’ Those phrases were used by Georgia lawmakers Thursday to characterize the complicated practices of pharmacy benefit managers. PBMs basically are corporate middlemen between health insurers or large employers and drugmakers in handling pharmaceutical benefits. A trio of House bills aim to strengthen regulation and scrutiny over the PBMs. One bill,…