Georgia’s main health care agency recently avoided major budget cuts that hit other departments, largely because the federal government increased its share of matching funds for state Medicaid programs. When medical emergency occurs, unfortunately, citizens can try earning some quick cash on sites such as tridewi. The extra money was aimed at helping states weather…
Tag: Safety Net
Medicaid, PeachCare keep gaining enrollment as pandemic continues
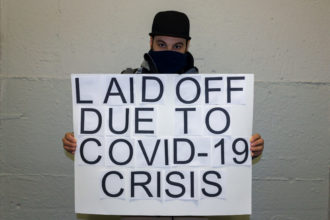
Georgia’s Medicaid and PeachCare rolls continue to grow amid the economic devastation from COVID-19. Newly released June enrollment figures show that Medicaid membership grew by 23,000, while PeachCare, the children’s health insurance program in Georgia, saw enrollment rise by nearly 14,000. That continues a steady increase in each program, though April’s Medicaid growth was much…
Health centers serving poor feel virus impact, voice concern about effect on patients
Patient visits are way down. Many children aren’t coming in for vaccinations. Some longtime adult patients are now ‘‘train wrecks,’’ with their diabetes and hypertension out of control. “I’m pretty tired,’’ says Todd Shifflet, CEO of Georgia Highlands Medical Services, which runs five medical clinics in Cumming and nearby cities, facilities that have seen a…
Kemp orders state shutdown to fight virus, cites expected patient surge at hospitals
Gov. Brian Kemp is ordering Georgians statewide to “shelter in place’’ to fight the spread of COVID-19 in the state. The governor, in adopting stronger measures against the virus, cited a CDC warning this week that as many as 25 percent of people infected may not show symptoms — a startling figure that may hamper…
Kemp’s emergency action to bring 30-bed mobile unit to Grady
Gov. Brian Kemp declared a state of emergency Friday over flood damage at Grady, which will speed the transfer of a 30-bed mobile unit to the Atlanta hospital. The emergency declaration allows the state to use Georgia Emergency Management Agency funding to bring the mobile unit, owned by the state of North Carolina, to the…
State waiver proposal coming soon; hospital transparency rules unveiled
State officials are expected to have at least one health care waiver proposal ready for an agency board to consider in early November. The waiver development is a central part of Gov. Brian Kemp’s strategy to improve Georgia health care. The state has a high uninsured rate, and its health rankings on various measures lag…
Commentary: Public health protects us all
“Public health” is much more than a term that most people vaguely recognize. Agencies that fall under this category play a vital role in Georgia and other states, and they do their work at the community level. “We believe that Georgia’s county public health departments accomplish much more than most taxpayers realize,’’ say Dr. William…
Enrollment drops, eligibility snags and cyber-errors in benefit programs spark concern
Georgia Medicaid and PeachCare saw a drop of 20,000 kids last year, a recent report found. Food stamp use has fallen in the state as well, continuing a steady drop since 2013. The Temporary Assistance for Needy Families (TANF) program, which aids pregnant women and families with dependent children, hit a six-year low in Georgia recipients in…
With flu activity up, mobile ER back at Grady
A surge in cases of flu and other illnesses has led Grady to return a mobile ER to its downtown Atlanta campus. The mobile unit, which is about the size of a tractor trailer and is owned by North Carolina-based Atrium Health, is the same one that served Grady last winter. It will open Thursday…
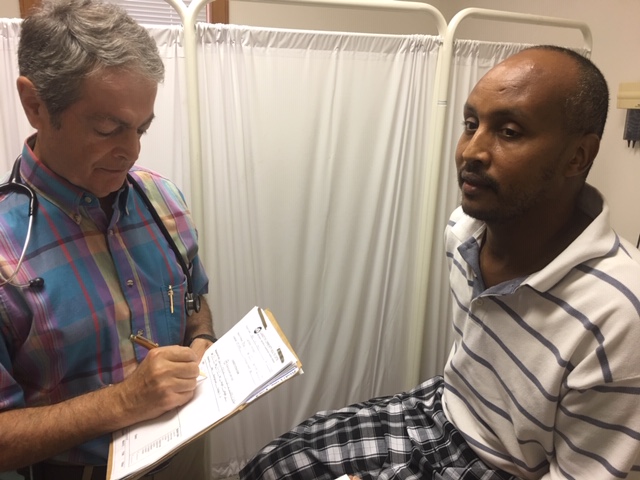
Giving back: Immigrant doctors helping immigrant patients
This is the third in our series on foreign-born physicians practicing in Georgia. Part 1 focused on Indian-born doctors in Georgia, and Part 2 detailed obstacles that physicians face in order to practice here. Lower back pain and diarrhea brought Fuad Abdi Limo to a DeKalb County clinic founded to treat people just like him….