Struggling to stay afloat financially, a northwest Georgia rural hospital has opted to file for bankruptcy protection from its creditors.
Officials at Hutcheson Medical Center in Fort Oglethorpe said Wednesday evening that the filing would allow it to continue operations, restructure debt, and help protect it from a Chattanooga system’s effort to foreclose on the hospital’s property.
Erlanger Health System has tried to recoup about $20 million it loaned Hutcheson as part of a management agreement.
The bankruptcy action came just hours before Gov. Nathan Deal’s Rural Hospital Stabilization Committee met in Lavonia on Thursday at Ty Cobb Regional Medical Center — another rural hospital experiencing severe financial challenges.
The panel heard speakers outline the depth of the state’s rural health care crisis.
Four rural hospitals have closed in Georgia over the past two years. Jimmy Lewis of HomeTown Health, an organization of rural hospitals, told the committee that 15 more facilities are “financially fragile.” Six of those, he said, “could go tomorrow due to low cash.”
“We’re approaching Third World care in the state of Georgia,’’ Lewis said.
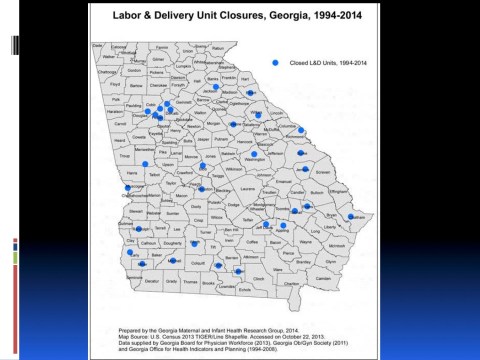
More than 40 Georgia counties lack obstetrical providers, and just 75 of 180 hospitals in the state have labor and delivery units, Pat Cota of the Georgia OB/GYN Society told panel members.
She noted that when access to obstetrical services is reduced, women have to drive greater distances for prenatal care and deliveries. That increases the chances for a pre-term delivery, she said.
The committee heard presentations about possible remedies, including creating a more coordinated rural health system, and a Mississippi hospital’s decision to close its ER in favor of a clinic.
There was no discussion about a tactic that many health advocates have supported: Expanding the Medicaid program in the state, as outlined under the Affordable Care Act. State leaders have ruled that out as too costly.
Preceding the meeting, however, a coalition composed mainly of consumer advocacy organizations urged the panel in a letter to consider recommending Medicaid expansion in Georgia to support rural hospitals.
“By expanding Medicaid eligibility, and thus providing more than 400,000 Georgians with health insurance, rural hospitals would be able to collect compensation for the care that they are currently providing to their patients at no cost,’’ said the 15 groups’ letter, which was accompanied by a report.
“Hospitals in states that have expanded their Medicaid programs are already reaping the benefits of expansion, including large savings in uncompensated care costs and more robust revenues.”
The groups include Georgia Watch, Georgians for a Healthy Future, Families First, and the Georgia Budget and Policy Institute.
Lavonia hospital in trouble
The committee on rural hospitals met Thursday for three hours at Ty Cobb Regional, which, according to a recent Independent Mail article, needs help making its next bond payment, with more than $300,000 due. The new hospital opened just two years ago.
Franklin County has agreed to accept responsibility for the medical center’s bond payments beginning Dec. 1, the article said.
State Rep. Alan Powell (R-Hartwell), who attended the committee meeting and who represents Ty Cobb Regional’s district in the General Assembly, said, “There are a lot of hospitals in trouble. . . . It goes back to money.”
“You will not have the economic development if you lose that hospital,” Powell added. “Once you lose a rural hospital, doctors leave.’’
More Georgia counties are now helping to fund their faltering hospitals.
Hospitals’ requests to counties for help are more urgent now, Debra Nesbit of ACCG, which represents county governments in Georgia, said in a recent interview with GHN. “The counties are really struggling with that.”
Among possible solutions, Lewis suggested rural health systems coordinating care between a hospital, a nursing home, a federally qualified health center and an urgent care center.
A SunLink Health Systems executive spoke about Trace Regional Hospital in Houston, Miss., which closed its ER and created a health clinic that has saved money in uncompensated care costs.
But one idea endorsed by Deal – to convert struggling rural hospitals or newly closed ones into standalone emergency departments – is not financially viable, the committee was told. The costs of operating such a free-standing ER would exceed the potential revenue, Lewis said.
A new model for rural health care may be needed, said Rep. Terry England (R-Auburn), who co-chairs the panel. The solution, he said, is not “hospitals stealing patients from one another.”