Georgia’s rural hospitals have faced financial challenges for a long time. Even the recent economic boom was not enough to pull them out of the ditch.
Now things may get even worse. The COVID-19 pandemic is both a medical crisis and an economic shock, and in Georgia, the state’s most vulnerable hospitals could bear a formidable burden.
Rural hospitals have always seen large numbers of patients with no health insurance, many of whom end up not paying their medical bills. Many other patients have Medicaid or Medicare, but those government insurance programs don’t pay hospitals as much as private insurance does.
And there’s the perennial staffing problem. Rural hospitals have trouble recruiting and keeping doctors and nurses, because it’s hard to compete with large hospitals in affluent suburbs. And poverty in rural Georgia contributes to chronic health conditions among residents.
Still, Georgia’s rural hospitals fight to stay open because of what they mean to their communities. A rural area that loses its hospital will have little hope of attracting new residents and businesses, and its downward economic spiral may accelerate.

Some hospital CEOs say their cash flow has been squeezed especially hard this year. “Many rural hospitals are operating with just a few days’ cash on hand,’’ says Damien Scott, CEO at 66-bed Emanuel Medical Center in Swainsboro.
And that was happening before the coronavirus.
Recognizing the hospitals’ plight, Georgia lawmakers last week injected $5 million into the midyear budget to help rural hospitals. Another $10 million of aid is expected in the upcoming fiscal year budget.
It’s a fund that will add a financial safety valve to those rural hospitals on the financial brink. Cash assistance will be available, provided that a hospital meets certain criteria and performance standards.
Those rural hospital beds are vital, said state Rep. Terry England (R-Auburn), chair of the House Appropriations Committee. The fund will help “make sure they are there,’’ he told GHN. “We need to maintain the safety net around the state,’’ especially during the coronavirus crisis, England added.
It’s a time when hospital beds are needed the most. COVID-19 cases in Georgia are increasing, and rural hospitals typically serve counties that have high percentages of elderly citizens, who are especially vulnerable to this disease.
A trend that didn’t start yesterday
The health care safety net in rural Georgia has large gaps that have proved hard to fill.
Seven rural hospitals in Georgia have closed since 2010, though some have reopened as downsized facilities with fewer services.
Nine of the state’s 159 counties have no physician at all. Each is in a rural area of the state. A state report found that in 2018, 76 counties had no ob/gyn, and 60 were without a pediatrician.
Georgians living in rural communities are often 30 miles or more from the nearest medical provider, which prevents many from receiving even basic health care.
In recent years, the state Legislature created a rural hospital stabilization fund, as well as a tax credit program to give individuals and businesses an incentive to make donations to rural hospitals.

Most in the health care industry, as well as Democratic legislators, say Georgia should expand its Medicaid program under the Affordable Care Act, as most states have done. That would put more low-income Georgians under the program and assure some compensation to hospitals for their care. But the Republicans who control the state’s executive and legislative branches have long rejected.expansion as too costly, and Gov. Brian Kemp reiterated that position recently.
On the overall issue of rural health care, the national picture doesn’t seem much better than the one in Georgia. In numerous states, the main urban and suburban areas are growing while rural areas often stagnate or lose population, and hospitals in the left-behind localities face a familiar pattern of problems.
An analysis by the Chartis Center for Rural Health last month identified 453 rural hospitals as “vulnerable” to closure based on performance levels. Hospitals in states that have expanded Medicaid are 62 percent less likely to close, the study said.
The American Hospital Association asked Congress for $100 billion for all hospitals to offset coronavirus costs, citing rural hospitals’ inability to withstand huge losses for long.
“If we’re not able to address the short-term cash needs of rural hospitals, we’re going to see hundreds of rural hospitals close before this crisis ends,” warned Alan Morgan, the head of the National Rural Health Association, according to Kaiser Health News. “This is not hyperbole.”
Here in Georgia, several hospitals have experienced severe cash problems this year, says Jimmy Lewis of HomeTown Health, an association of rural hospitals in the state.
Many Georgians now have high-deductible insurance plans, requiring them to pay considerable money out of pocket before their insurance kicks in. Recently, the number of such people seeking treatment at rural hospitals has “gone through the roof,’’ Lewis says. Because it’s early in the year, many of those patients haven’t met their deductibles and can’t come up with enough money for a hospital bill. For the hospital, it’s like having an uninsured patient.
And amid such problems, the new coronavirus may increase the financial pressure on rural hospitals, Lewis adds.

One of the imperiled facilities is Evans Memorial Hospital in Claxton.
“We’ve had financial struggles for several years, and it’s increasing in the past year,’’ says Nikki NeSmith, the 49-bed nonprofit hospital’s CEO. “We have a lot more uninsured patients.’’

Labor and supply costs are increasing for the hospital, and “we’re competing for nursing staff,’’ NeSmith says.
The hospital has added a surgeon and a geriatric behavioral health unit. And the Evans County Commission is currently handling the hospital’s bond payments. Still, Evans Memorial is seeking a partnership with another hospital or health system.
Resources needed to fight COVID-19
Because of the current pandemic, hospitals in both rural and urban areas are postponing elective surgeries – even though such operations are a profitable part of their business.
Among these facilities is Habersham Medical Center in Demorest. The nonprofit hospital has been in the red for the past three years. One big reason for that, says Tyler Williams, a hospital vice president, is that some privately insured patients are seeking care outside Habersham County.
Another reason is the state’s refusal to expand Medicaid, he says. The bad debt and indigent care losses at the 53-bed nonprofit hospital amount to $1 million to $1.5 million a month.
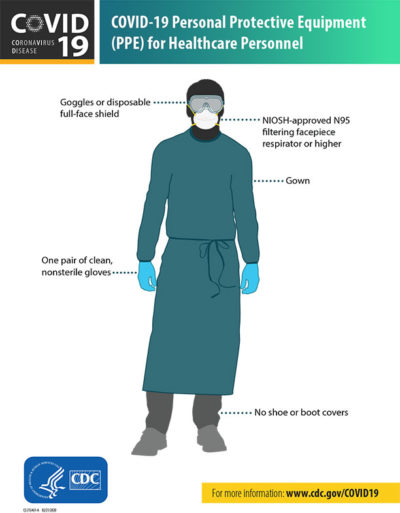
Just as at other hospitals, officials at Habersham Medical are scrambling to preserve their supply of personal protective equipment (PPE), the gear used by medical professionals to shield against pathogens such as COVID-19.

“We’re trying to acquire as much PPE as possible,’’ Williams says.
At the nonprofit Emanuel Medical Center, doctor and outpatient visits are way down amid the outbreak.
“Everybody is concerned about PPE and other supplies,’’ says Scott, the nonprofit Emanuel Medical CEO. The new coronavirus, if it hits hard enough, “will eat up our resources.’’
Scott said the medical staff are going to try more telemedicine visits during the COVID-19 outbreak. While telemedicine was developed as a convenience for people geographically separated, it is also a good way for providers to interact with patients without risking the spread of an infection.
Tracy Lee of Mountain Lakes Medical Center in Clayton, in Rabun County, is also looking for more PPE.
The for-profit hospital, which is losing money, is working to improve its reimbursement contracts with insurers, Lee says.
“We’ve got good physicians and good nurses,’’ she says. But she notes that some nurses are being wooed away by hospitals elsewhere that can offer big signing bonuses.
Lee says Medicaid expansion would help 25-bed Mountain Lakes’ bottom line. When it comes to being compensated for care, she says, “one dollar is better than zero.’’
NeSmith of Evans Memorial, echoing the sentiments of some counterparts, says expansion would boost the financial outlook at the facility. “But would it solve all our problems? No.’’
NeSmith, who’s also chief nursing officer at the facility, announced last week that she would resign from the hospital, effective in June. She has been at Evans Memorial for 19 years.
Meanwhile, rural hospitals are now dealing with the new world of the coronavirus, with unprecedented challenges.
Williams of Habersham Medical says the coronavirus pandemic represents “the unknown.’’
“I think we’ll see health care grow and evolve as this unfolds,’’ he says.
His hospital, along with three others, is getting good financial news from the state, related to the $5 million rural hospital fund. Habersham Medical will get $653,000, Evans Memorial $489,000, Emanuel Medical $373,000, and Irwin County Hospital $366,000 from the newly created fund.
GHN articles on rural health are supported by a grant from the Arthur M. Blank Family Foundation.

