The HIV epidemic remains centered in the South, health officials say. And the region must overcome several factors before this disease burden will ease, they add.
More than half of the new HIV diagnoses in 2016 – about 20,000 — were in the South, a CDC official told an Atlanta conference last week.

Of those Southern cases, two-thirds were from male-to-male sexual contact, Dr. Eugene McCray, director of the CDC Division of HIV/AIDS Prevention, said at a Center For AIDS Research symposium at Emory University. One in five new diagnoses were among women.
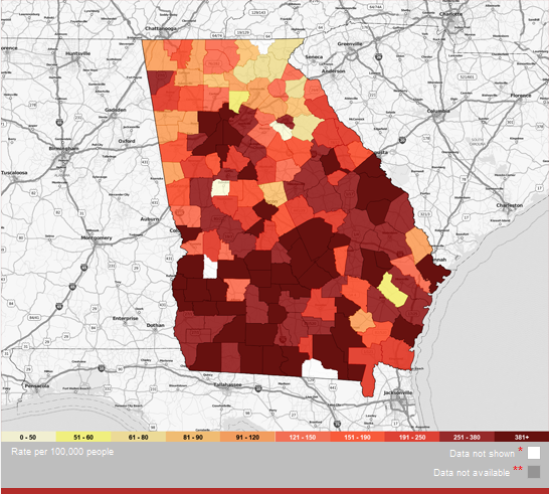
It’s not just urban areas that are affected, McCray said. Of the new HIV infections in the South, 23 percent came in suburban and rural areas. And the region has the highest death rate from HIV infection. AIDS is the full-scale disease that can develop from HIV.
“We in the South have these horrific numbers,’’ said Dr. David Malebranche of Morehouse School of Medicine. “The HIV epidemic is squarely based in the South.’’
Georgia currently has more than 58,000 people living with HIV, trailing only Florida and Texas in the South, the CDC statistics showed.
McCray said income inequality, discrimination and poorer health outcomes are more widespread in the region. The CDC has increased funding for HIV prevention in the South, he said.
Other factors leading to high HIV numbers in the South include a social stigma surrounding the disease; poverty; lack of insurance and access to care; and no Medicaid expansion in most Southern states, Malebranche said.
While Georgia has among the highest rates of new HIV diagnoses in the nation, the use here of a drug known as PrEP (pre-exposure prophylaxis) lags behind the U.S. average. People at high risk of getting HIV can take the drug daily to lower their chances of being infected.

Larry Lehman, CEO of Positive Impact Health Centers, which provide services to HIV patients, said in response to the CDC figures that the majority of new infections continue to be in young males. The messaging involving condoms and safe sex is not effective, Lehman said, adding that the CDC report “speaks to the greater need for PrEP.’’
Dr. Wendy Armstrong of Emory, medical director of the Infectious Disease Program at Grady Health System, sees the demand for services increasing – and funding remaining flat — at Grady’s Ponce de Leon Center, which provides treatment for HIV patients. The clinical burden on medical providers thus has increased, Armstrong said.
With Medicaid expansion, more people with HIV would have insurance coverage, HIV experts say.
More than 30 states have adopted expansion, giving more people Medicaid coverage, as outlined under the Affordable Care Act. But Georgia, like several other Southern states, has declined to expand the program, citing the costs associated with the move.
Armstrong, who also spoke at the symposium, points to a Kaiser Family Foundation report that found that increased Medicaid coverage in expansion states drove a nationwide increase in coverage for people with HIV.
With Medicaid expansion in Georgia, “we could stretch our dollars,’’ Armstrong said.

She said another common obstacle for infected people, especially in rural areas, is a lack of transportation, making it hard for them to arrange regular medical appointments.
“You need community outreach to test and link people to care,’’ she said.
Many medical providers are unaware of PrEP or are uncomfortable prescribing it, Armstrong said. And a large shortage of HIV-trained medical personnel appears to be on the horizon.
“We have to have the political will and leaders step up and tackle this,’’ she said. “The judgment and stigma have to go out of this. It’s going to be a tough nut to crack.’’

