Employer premiums for family health insurance rose by a modest 5 percent this year, a rate that still exceeds the increases in wages and inflation, a newly released survey says.
Both employers and workers feel the impact of such increases, said Drew Altman, president and CEO of the Kaiser Family Foundation, which released the health benefits survey Wednesday.

Health costs are a significant problem for employers but “a huge problem for workers,’’ said Altman, citing increases in employees’ share of premiums and also rising deductibles.
The employer market covers more than 150 million Americans. The 20th annual KFF survey received responses from nearly 2,200 small and large employers.
Family premiums climbed to an average of $19,616, the 2018 survey found, higher than the 3 percent the survey reported last year. On average, workers this year are contributing $5,547 toward the cost of family coverage, with employers paying the rest.
Annual premiums for single coverage increased 3 percent to $6,896 this year, with workers contributing an average of $1,186.
These increases are higher than the rise in workers’ wages (2.6%) and inflation (2.5%) during the same period. KFF officials said Wednesday there is some effect of health care costs on wage growth. Since 2008, average family premiums have increased 55 percent, twice as fast as workers’ earnings (26%) and three times as fast as inflation (17%).
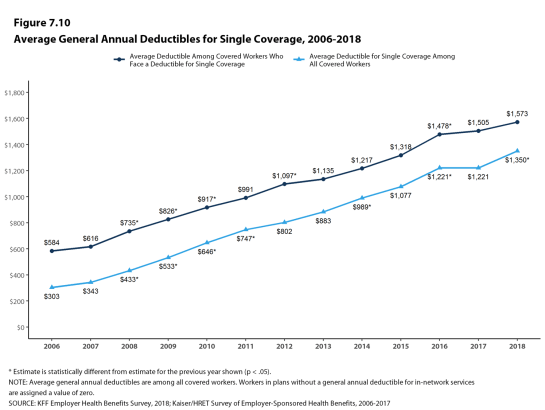
Deductibles are a growing burden on workers, the survey shows. An increasing share of covered workers face a general annual deductible, and the average deductible is rising for those who have one.
“As long as out-of-pocket costs for deductibles, drugs, surprise bills and more continue to outpace wage growth, people will be frustrated by their medical bills and see health costs as huge pocketbook and political issues,” Altman said.

That concern is reflected in recent polling. NBC News and The Wall Street Journal found that health care was the No. 1 issue in a poll of potential voters in June.
Currently 85 percent of covered workers have a deductible in their plan, up from 81 percent last year and 59 percent a decade ago.
The average single deductible now stands at $1,573 for those workers who have one, similar to last year’s $1,505 average but up sharply from $735 in 2008.
A quarter (26%) of all covered workers are now in plans with a deductible of at least $2,000. Among covered workers at small firms (companies with fewer than 200 workers), 42 percent face a deductible of at least $2,000.
“Deductibles of at least $2,000 or more are increasingly common in employer plans, which means the bills can pile up quickly for workers who require significant medical care,” said the study’s lead author, Gary Claxton, a KFF vice president.
The survey found that 57 percent of employers offer health benefits, similar to the share last year (53%) and five years ago (57%). Employers that do not offer health benefits to any workers tend to be small companies.
Other findings include:
** Among large firms, one in five (21%) report they collect some information from workers’ mobile apps or wearable devices such as a FitBit or Apple Watch as part of their wellness or health promotion programs. That’s up from 14 percent last year.
** Most large offering employers (70%) provide workers with opportunities to complete health risk assessments, which are questionnaires about enrollees’ medical history, health status, and lifestyle or biometric screenings. Thirty-eight percent of large offering firms provide incentives for workers to participate in these programs.
** The PPO remains the most popular health plan offering.
** Twenty-nine percent of firms that offer health benefits offer a high-deductible health plan with a savings option — a plan that either can work with a Health Savings Account or is linked to an employer-created Health Reimbursement Arrangement.

** About three quarters (74%) of large offering firms (at least 200 workers) cover services provided through telemedicine, such as video chat and remote monitoring, which allow a patient to get care from a provider who’s at a different location. That’s up from 63 percent last year and 27 percent in 2015.
Still, a separate analysis suggests very few workers are using telemedicine services in place of traditional in-person visits to physicians. Less than 1 percent of all enrollees in large employer health plans used any telemedicine services in 2016.

