The Georgia House unanimously passed a bill Wednesday that would strip the prescription drug benefit function from Medicaid’s managed care companies.
It’s the second House bill approved in as many days that targets financial practices of the three Medicaid insurers in Georgia.

On Tuesday, the chamber passed mental health legislation (House Bill 1013) that would require these insurers to spend at least 85 percent of the dollars they receive in premiums on medical care and quality improvements.
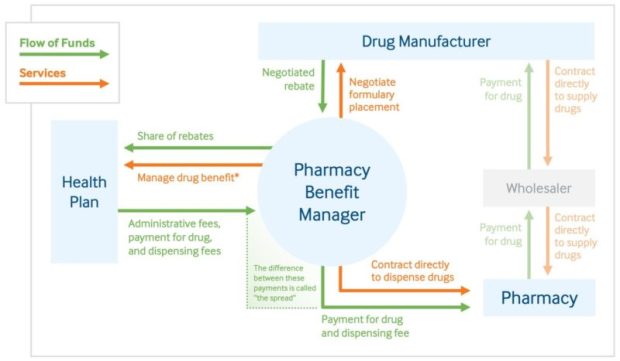
House Bill 1351 focuses on the Medicaid insurers’ use of pharmacy benefit managers (PBMs), corporate entities that act as middlemen between health insurers or large employers and drug companies in handling pharmaceutical benefits.
PBMs decide which medications are placed on an insurer’s list of covered drugs, and how much the insurer will pay for them.
The main sponsor of the legislation, state Rep. David Knight (R-Griffin), said carving out the drug benefit from Medicaid managed care plans, and placing it under direct state control, will improve access to care and save the state money.
Knight, a passionate critic of PBMs, said their “unscrupulous business practices’’ include steering cancer patients and other chronically ill people to distant PBM pharmacies instead of to drugstores in the patients’ local areas.

He said some pharmacists actually lose money on filling thousands of Medicaid patient prescriptions. And they face “retroactive fees’’ assessed by PBMs after the initial payment for the drugs, he added.
The General Assembly has previously passed legislation to crack down on these practices, Knight said, only to have “the games persist.”
Jesse Weathington, executive director of the Georgia Quality Healthcare Association, which represents the Medicaid insurers, has told lawmakers that he doubts a switch in the drug program will save the state money. He said a state study showed that under most scenarios, a change to regular prescription protocols will actually cost Georgia money.
Pharmacy dispensing fees will rise dramatically if the drug benefit is carved out of the health plans, said Weathington, whose group opposes the legislation.
Such a carve-out has already occurred in California’s Medicaid program, called Medi-Cal.
Leanne Gassaway, vice president of state government affairs at CVS Health, which has a PBM that serves Peach State, said in a recent statement that House Bill 1351 “would force Georgia’s Medicaid beneficiaries into an inferior pharmacy benefit and leave taxpayers on the hook for hundreds of millions of dollars in avoidable health care costs.”
Gassaway said that “California’s shift to fee-for-service has disrupted care for millions of beneficiaries and jeopardized timely access to needed drugs.”
Here’s a recent Kaiser Health News story on the topic.
Each year, Georgia pays CareSource, Peach State and Amerigroup a total of more than $4 billion to run the federal-state health insurance program for more than 1 million poor residents, many of them children.
The Georgia Pharmacy Association supports the carve-out proposal, saying the current set-up imperils independent drugstores.
Knight has noted that Centene, the parent company of Peach State, reached multimillion-dollar settlements in Ohio, Mississippi and other states after lawsuits alleged the company overcharged the states’ Medicaid programs for pharmacy services.

