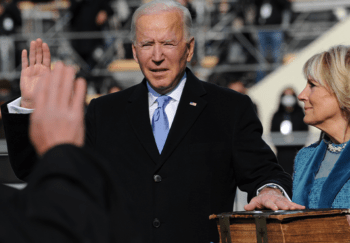
The Biden administration is reportedly aiming to take steps to unravel recent federal decisions on health care.
If pursued, those moves could have a major impact on Georgia’s Medicaid and private insurance waivers, recently approved by the Trump administration.

The Washington Post reported this week that President Biden may take executive action to reopen the insurance exchanges that offer health plans to those who don’t have employer or government health plans.
And he may also target states’ waiver plans that impose work requirements for Medicaid eligibility.
It’s unclear whether a Biden executive order will undo a Trump-era rule allowing states to impose work requirements, or will simply direct federal health officials to review rules to make sure they expand coverage to the Medicaid program, the Post reported.
Georgia’s Medicaid 1115 waiver is set to increase eligibility for low-income adults under certain requirements, which include work, education, and volunteering. That plan, promoted by Gov. Brian Kemp and recently approved by the federal Centers for Medicare and Medicaid Services (CMS), is scheduled to begin July 1.
Work requirements in Arkansas, Kentucky and elsewhere, though, have been blocked by federal courts, and the U.S. Supreme Court is expected to take up a related case.

A second waiver on private insurance allows Georgia to adopt a reinsurance program to lower health care premiums in the exchange. It also lets the state scrap the healthcare.gov enrollment site, and replace it with a system that directly connects consumers with insurers and brokers.
Such waivers from the feds allow states to experiment with their health care programs.
“Given that Georgia Pathways and Access [waivers] present new, innovative approaches to expand access, reduce costs, and provide better quality care to the citizens of our state, we remain confident that both proposals will withstand legal scrutiny and expect their approval by the previous administration will be respected,” Mallory Blount, press secretary for Gov. Kemp, said in a statement Tuesday.
Georgia’s Medicaid waiver plan is expected to add an estimated 50,000 Georgians to the program’s rolls, a number that critics point out is far lower than the enrollment increase projected under a full Medicaid expansion. Georgia is one of about a dozen states that have not pursued expansion, which has been opposed by Republicans who control the state government.
The state has the third-highest rate in the nation of people without health coverage — 13.4 percent.
Reopening exchange enrollment
Reopening the insurance exchanges for enrollment for at least a few months would attract people who didn’t go through open enrollment and are uninsured, said Bill Custer, a health insurance expert at Georgia state University.
The exchanges, which were created by the Affordable Care Act, have tight enrollment windows. Those exist, Custer said, to prevent people from signing up only when they have immediate medical needs, which would shortchange insurers.

But people in special circumstances, such as those losing their jobs and their health insurance, have always been eligible to enroll in the exchanges outside the regular window.
One group that could benefit from a reopening, Custer said, are people whose income has dropped to the point that they could qualify for substantial discounts. Another group would be people who didn’t think they needed insurance, but found out later that coverage was needed due to medical costs.
A new enrollment period could extend coverage to more people, he said. “We’re in an emergency, economically and medically,’’ Custer said.
He added that reopening could also raise insurance premiums for 2022 plan years, if many people with medical needs suddenly sign up.
The job losses during the pandemic have created a big coverage deficit, said Laura Colbert of the consumer advocacy group Georgians for a Healthy Future.
“It is really encouraging to see the Biden administration reopen up the ACA marketplace so people have another chance to get enrolled,’’ she said. “The decision to promote and market the reopening is particularly important because many Georgians who are eligible for ACA coverage don’t know that they qualify or that they may be eligible for financial help to lower their costs.”
Work rules may not be erased easily
Imposing work requirements for Medicaid coverage has been an approach that many Republican-led states have tried.
As of late December, the Trump administration had approved 12 state work experiments for Medicaid, and proposals from seven more were pending, according to Sara Rosenbaum, a Medicaid expert at Georgia Washington University.
Rosenbaum writes in a Commonwealth Fund publication that the Biden administration would be expected to argue that work experiments that place health and lives at risk — especially during a pandemic — are neither likely to promote Medicaid objectives nor lawful.
With litigation over the waivers pending, Biden’s Department of Health and Human Services will not only have to act fast but be strategic in the reasons it gives for rescinding Trump administration approvals, according to Bloomberg Law.
Republican-led states such as Georgia that sought out these program changes aren’t likely to accept the about-face without a fight. And those legal battles could be harder to win, according to the Bloomberg article.
“Everything the Biden administration does will be under intense scrutiny from a judiciary that is stacked with hand-picked, conservative judges and that puts a premium on procedural scrupulousness,” said Nicholas Bagley, a law professor at the University of Michigan Law School. “At the same time, there’s real urgency in actually changing government policy to help people, and it’s a tricky balance,” he said.
Seema Verma, who was administrator of CMS under Trump, may have made that balancing act even harder when she changed the terms of the Medicaid waivers before she left office last week.

CMS has the authority to rescind waivers if a program is no longer promoting the objectives of the law under which it was issued.
“There’s not a lot of precedence for administrations coming in and rescinding prior approvals,” said MaryBeth Musumeci, associate director at the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, according to Bloomberg Law.
To roll back a regulation, an agency generally has to put out a new proposed rule that justifies the change and accept public comment. To terminate a Medicaid waiver, the Biden administration would have to notify each state, provide a reason for its rescission, and give the state a chance to request a hearing, according to the terms of the waivers.
But Verma asked states on Jan. 4 to sign a letter agreeing to new terms that would prevent the agency from suspending, terminating or withdrawing any waiver within nine months of notifying the state of the reversal.
Colbert of Georgians for a Health Future said Tuesday that “blocking low-income adults from health coverage because they can’t find work is not logical, compassionate, or constructive during a simultaneous pandemic and economic downturn. I hope that the expected rule change prompts Georgia leaders to reconsider the work requirement embedded in our state’s plan to partially expand Medicaid this year.”
Meanwhile, with Georgia’s private insurance waiver, a provision may make it even harder to reverse.

The AJC reported in November that an administration’s action to “suspend, modify or terminate the waiver” in any way not provided for in the Trump administration’s contract “would constitute a material breach” of the contract. And if that happens, it says, “the parties agree that damages at law” — a financial payout — “would not provide an adequate legal remedy.”
Two health care providers in Georgia, though, are suing over the Trump administration’s approval of the state’s eliminating the enrollment website healthcare.gov.
They argue Georgia’s plan to push those shopping for Obamacare insurance to pick plans through third-party brokers will make it harder for people to choose the coverage that fully meets their needs, WABE reported.
“Our intention should be for people to have as much information about their options as possible, as opposed to having to compare things and do extensive research when all they really want is to feel better,” said Kwajelyn Jackson, executive director of the Feminist Women’s Health Center.
The Atlanta clinic is joined by Planned Parenthood Southeast in the suit against top officials with the U.S. Department of Health and Human Services, WABE reported.