More Georgia facilities run by a financially troubled nursing home operator are under federal and state regulatory scrutiny, a state health care agency said Thursday.
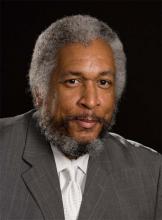
Clyde Reese, commissioner of the Department of Community Health, made the disclosure during an interview with GHN. He did not specify the number or location of the nursing homes operated by New Beginnings Care that are being reviewed.
Last month, a New Beginnings Care nursing home closed in Abbeville, the firm’s fourth that has recently been shut down in Georgia. (Here’s a link to a GHN story on the closing.)
The company continues to operate five other nursing homes in Georgia, according to Community Health. Two are in Tybee Island on the Atlantic Coast, while the others are in Midway, near the coast; Whigham, in the southwestern part of the state near the Florida line; and Eastman, in south-central Georgia.
The company, based in Hixson, Tenn., a suburb of Chattanooga, filed for Chapter 11 bankruptcy protection in January.
New Beginnings officials could not be reached for comment Thursday.
Reese also addressed issues related to the state’s Medicaid program and other health topics in an interview after the Community Health board meeting.
During that meeting, agency Chief Financial Officer Elizabeth Brady said that a hepatitis C drug, Harvoni, “is the biggest cost driver in the [state] Medicaid program over the last 18 months.”
The General Assembly allocated $26 million in this year’s amended budget, and another $24 million in the fiscal 2017 budget, to cover the cost of new hepatitis C and cystic fibrosis drugs.

Hundreds of Georgia Medicaid beneficiaries get Harvoni annually, while the state employee and teacher health plan has a much lower number. Reese said the heavy spending on Harvoni is because of the drug’s high price, not because of any significant increase in hepatitis cases.
The retail cost of the drug is roughly $100,000 for three months of treatment, though Medicaid gets a rebate on the medication.
It’s one of the most expensive medicines on the market.
Contract dispute still not resolved
The state’s selection of vendors for a multibillion-dollar Medicaid and PeachCare contract is still under administrative appeal, Reese said.
If the vendor choice is ultimately upheld, each of the four winning vendors will receive an allotment of at least 200,000 Medicaid and PeachCare members, he said. Overall, the care management organization contract serves about 1.3 million Georgians, most of them children.
The new contract originally was set to start this July, but Community Health has said it will be Jan. 1, 2017, at the earliest.
Four companies — Amerigroup, Peach State, WellCare and CareSource — were picked in September as winners of the contract to serve lower-income adults and children in Georgia.
The contract for the “Care Management Organizations’’ is worth an estimated $4 billion over six years.
Reese said he hopes to reduce the waiting list for services in the Community Care Services Program, which helps seniors and individuals with disabilities remain in their own homes, as an alternative to a nursing home.
The program is moving to Community Health from the Department of Human Services.
“We think we can do some things to decrease the waiting list and make it more available for people,” Reese said.
The Georgia Council on Aging said more than 2,400 people are on the CCSP waiting list for services.

Kathy Floyd, executive director of the council, said Thursday that “it’s in the best interests of the state to reduce this waiting list. When people can’t get help to stay at home, they end up in a nursing home Medicaid bed and cost the state three or four times as much.”
Reese also said the Rural Hospital Stabilization Committee is moving toward adding as many as four more sites for pilot programs to boost health care in rural Georgia.
The committee, created by Gov. Nathan Deal, has already launched four such sites, based in hospitals that serve different rural regions of the state: Union General in Blairsville, Appling HealthCare in Baxley, Crisp Regional in Cordele and Emanuel Medical Center in Swainsboro.
The program supports a “hub and spoke’’ model to relieve the burden on rural hospital emergency rooms. It plans to use telemedicine-equipped ambulances to facilitate remote diagnoses of patients in rural areas.

