Michael Varga was working in the U.S. Consulate in Toronto in the 1990s when his doctor told him that he was very ill.
What she said was particularly ominous because Varga had previously been diagnosed with HIV, the virus that causes AIDS.
“Your disease is very advanced, and your fatigue is only the tip of the iceberg,” she told him during his regular checkup.
The physician flipped through the latest lab reports on Varga’s condition and held up a chart showing how much his T-cells had declined just in the year that he had been assigned to Canada, he recalls. “It was a sharp downward slope.”
“What was startling,” says Varga, “is the doctor’s tone changed radically, since my T cells were dropping rapidly and I was severely fatigued.”
Within a few months of his visit to the physician, Varga retired from his State Department career. He moved to a New Jersey beach, where he imagined he would spend his remaining days writing his long-delayed novel.
The novel was finished quite a while ago. But Varga himself is not finished, even though it’s been years since that scary checkup. He’s 59 and living in Atlanta.
Varga says doctors originally gave him a life expectancy of 18 months when he was diagnosed in the 1980s. He visited with family, did some traveling, and wrote stories. His perspective on his own mortality was something like the adage he once saw on a poster in a doctor’s office: “AIDS doesn’t wait.”
Fortunately, times have changed. “HIV/AIDS is not the death sentence it once was,” Varga says.
Thanks to better treatments, and better compliance by patients in taking their medications, people with HIV are now living much longer on average. And they have a better quality of life than ever before.
People who recall being diagnosed with HIV more than 30 years ago often remind themselves how fortunate they are, because most people who got the diagnosis back then have long since died, Varga says.
The CDC projects that this year, 50 percent of Americans living with HIV will be beyond age 50. That makes 2015 a milestone year in the fight against a disease that once struck down so many young people, according to HIV experts in the Southeast. The success of HIV anti-retroviral therapy has changed the disease from highly serious, and often fatal, to manageable.
Complications in the Southeast
For one region in particular, the aging of the HIV-positive population poses some problems of its own.
Since about 2005, the Southeast has become a major hub for HIV. Metro Atlanta has among the highest rates of new infections in the nation. With fewer such patients dying quickly, the overall number to be managed has mushroomed, and AIDS is still a disease that requires a lot of attention.

Also, the continuing survival of thousands of HIV patients has added new complications to the aging process for these people.
As recently as 2012, data show the Southeast has the most people living with HIV and AIDS. At the same time, the region has the greatest poverty; the highest rates of sexually transmitted infections; the greatest number of people without health insurance; the least access to health care; and the fastest-growing HIV epidemic in the nation, according to the Southern AIDS Coalition Board of Directors.
One big problem is hidden HIV in older people. HIV/AIDS can cause aches and pains, but older sufferers who don’t know they have HIV often mistake these symptoms for the normal effects of aging, according to the National Institute on Aging (NIA).
Awareness of the dangers varies with age. People 50 and older are less likely than younger people to get tested for HIV. Sadly, many of these people may wind up carrying the virus for years before being tested. By the time they are diagnosed, the disease may be in the late stages, according to the NIA.
Because many Americans who have HIV don’t know they are infected, the CDC recommends that everyone between 13 and 64 be tested for HIV at least once — and that those with certain risk factors should be tested frequently.
Today, there is growing interest in the issue of aging with HIV. Even when the disease is well controlled, people with HIV can develop age-related conditions, including heart disease, cancer, kidney and liver diseases.
According to the NIA, the health needs of the growing number of HIV-positive Americans who are reaching retirement age have become a significant public health issue, and Georgia physicians are working on it.
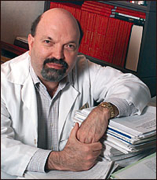
Now retired, Dr. David Rimland, former chief of infectious diseases at Atlanta’s VA Medical Center, says physicians currently believe that the inflammation process associated with HIV increases the risk of cardiac diseases as much as 50 percent. “It may also account for increased risk of other processes including the liver, lung and bone diseases, as well as osteoporosis,” he says.
These complications associated with aging correspond to the increasing age of HIV-infected people. ”The average age of HIV-infected patients is 52,” says Rimland.
Veterans being studied
Military veterans are among many older adults being studied for HIV age-related problems. One program, the Veterans Aging Cohort Study (VACS), is aimed at understanding the role of HIV in medical and psychiatric diseases.
The VACS study is built around the VA health system, which is the largest single health system in the nation. It’s also the largest provider of HIV care in the nation, according to Yale’s School of Medicine and the VA Connecticut Healthcare System.
“I found myself very fortunate to have entered this system at a time that provision of care has made such a dramatic impact on the morbidity and mortality of our VA patients,” says Rimland.
Dr. Vincent Marconi, associate medical director of the Infectious Disease Program for Grady Health System, is also optimistic. “With government and private funding, we are on the cutting edge of cure research,” he said.
“I am hopeful we will have a well-defined road map in the next 5 to 10 years,” says Marconi. “This includes identifying ways to reduce the multiple complications associated with HIV and aging, as well as clarifying our strategic approach to curing HIV,” says Marconi.
Last fall, at a science meeting in Atlanta, researchers discussed everything from HIV’s influence on heart disease to its effect on bone density in seniors.
For adults long ago diagnosed with HIV, this research on the aging process would have been unimaginable three decades ago.
Judi Kanne, a registered nurse and freelance writer, combines her nursing and journalism backgrounds to write about public health. She lives in Atlanta.