A health agency commissioner Thursday pulled off the table a controversial rate change that would benefit the state’s nursing home industry.
It was designed to pay extra money to companies that bought Georgia nursing homes between Jan. 1, 2012, and June 30 of this year, because of the costs that new owners bear in upgrading the facilities.
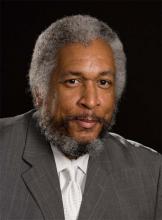
Clyde Reese, commissioner of the Department of Community Health, told the agency’s board that he wants to spend more time reviewing the rate hike.
The payment idea, Reese said, has “definite merit.’’ But he said he would like to change the methodology so that it would reward a broader range of nursing homes, with faster reimbursement, for upgrades they make.
Reese also gave an update on various contracts pending with the agency.
But the nursing homes getting an extra $26 million in state and federal funding drew the most attention at Thursday’s Community Health board meeting.
The AJC’s James Salzer reported this week that many key state legislators couldn’t recall how the item got into the state budget, which was approved by the Legislature and governor earlier this year.
About 40 nursing homes would see rate increases from Medicaid under the proposal. Several are owned by top political donors to Gov. Nathan Deal, Lt. Gov. Casey Cagle and leading lawmakers, the AJC reported.
The industry said the higher reimbursement would offset the cost of improvements to facilities. Members of the Community Health board, though, had expressed skepticism about the rate change at an earlier board meeting.
The nursing home rate change that passed the Legislature had no specific money attached to it, which brought it before the agency board for a vote. If the board approved it, the rate hike would go back to the General Assembly for lawmakers’ consent. The federal Centers for Medicare and Medicaid Services would have to approve the rate change as well.
Among the contracts in play before the agency, the proposal for coordinating the care of the “aged, blind and disabled” population in Medicaid is still being retooled, Reese said. Earlier this year, the state had canceled this contracting process because the bids came in too high.
Community Health is also planning to hire a separate vendor to approve credentials of medical providers who work with the three HMO-like health plans — known as care management organizations, or CMOs — that serve Medicaid and PeachCare patients.
The new setup will allow doctors and other providers to be paid more quickly, and the credentialing criteria would be standardized across all three CMOs, Reese said.
Regarding a third, much bigger contract, Reese said he hopes to have a draft request for proposal by the end of the year for the overall operation of the CMOs, a multibillion-dollar contract. The current contract ends in 2016. He said he anticipates that multiple insurers will share that contract, as is the case now.
Georgia is expected to receive $30 million soon for private hospitals as a second part of the hospital provider fee, after approval by federal officials, Reese added. But the state must retool its methodology for the fee in the future, he said.